Food is Medicine Community Action Plan
The Food is Medicine Community Action Plan builds on Food & Society at the Aspen Institute's Research Action Plan by translating the evidence for Food is Medicine into practical, community-driven strategies that improve health, strengthen local food systems, and advance equity. Developed through multi-year convenings with clinics, community organizations, food producers, researchers, payers, and program implementers, the Community Action Plan highlights real-world innovations, elevates what works in diverse settings, and offers actionable guidance on designing, funding, evaluating, and scaling Food is Medicine interventions.
Centering community is essential. Food is Medicine programs succeed only when they reflect the lived experiences, cultural foodways, economic realities, and structural barriers of the people they aim to serve. When community voices shape design and governance, programs are more trusted, accessible, and sustainable, and they yield stronger health outcomes—bridging Food is Medicine as a clinical intervention with a community-anchored movement for long-term well-being and food sovereignty.
Food affects our physical and emotional health. In the U.S., there is a growing conversation about how best to incorporate food in our health care as a potent healing or preventative intervention. The phrase “Food Is Medicine” has become shorthand for a set of practices that intentionally apply food to prevent, manage, treat, or reverse disease. Food is Medicine may seem to be a new trend, but there is a meaningful history of Food is Medicine work by communities. For many years, communities have developed and implemented innovative initiatives to provide healthy meals and groceries to people experiencing health challenges. These initiatives' successes have led health care systems, payers, and policymakers to look for ways to scale Food is Medicine to serve more people. Increased interest-and the potential for increased investment-has created a Food is Medicine landscape where community-engaged initiatives share space with large established businesses and new technology-based companies. The guide you are reading exists to remind readers of the broad range of community-based organizations and community champions working in Food is Medicine, to highlight the valuable contributions they make, and to explore why and how funding can flow to them.
Why Food is Medicine?
People in the United States eat a lot of unhealthy food. If there were such a thing as the average diet for an average person in the U.S., the diet would include many ultraprocessed foods and fall well short of doctors' and scientists' recommendations. At the same time, many people in the US worry about their households' ability to afford enough food. Around 13% of U.S. households in 2023 reported food insecurity at some point in the last year, meaning they had difficulty providing enough food for the household due to a lack of resources. Many of the people reporting food insecurity-and others who did not report food insecurity-would also meet the criteria for nutrition insecurity. People experiencing nutrition insecurity have difficulty consistently accessing affordable foods that promote health and prevent or treat disease.
Read More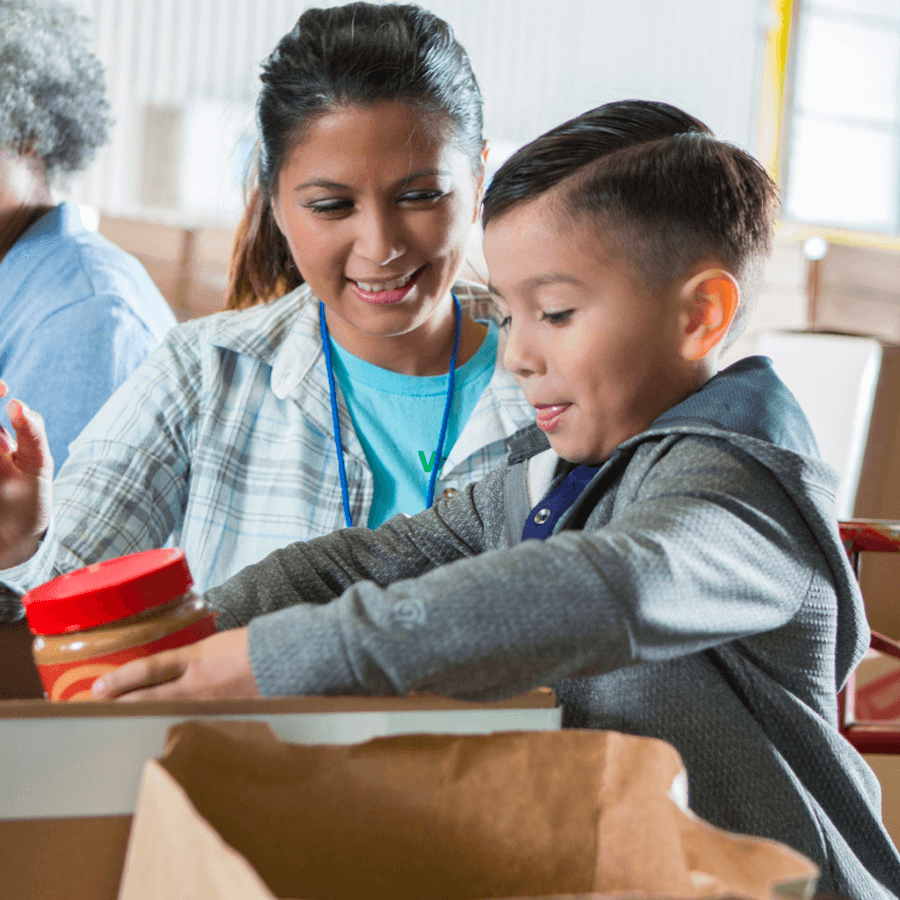
Why Focus on Communities?

Community-based organizations (CBOs) have been responsible for implementing Food is Medicine interventions for decades. As far back as the 1980s, community-based organizations across the U.S. led the way in implementing the home delivery of meals and groceries to people living with HIV/AIDS. Community-based organizations soon began to provide food services to people living with cancer, heart disease, and other conditions. Community-based organizations -particularly faith-based organizations-have also taken on much of the challenge of distributing food to people experiencing food insecurity.
Read MorePerspectives From the Field
A series of one-on-one interviews was conducted with representatives from five community-based organizations and six health care payer organizations, with the overarching purpose of identifying challenges and opportunities for Food is Medicine collaborations between community-based organizations and health care. Semi-structured interview guides-one for each group-were co-developed by Food & Society at the Aspen Institute and the Center for Nutrition and Health Impact. For the purposes of these interviews, we defined community-based organizations as regional or local organizations that provide medically-tailored meals, provide medically-tailored groceries (which includes some food banks and charitable food system organizations), or administer a produce prescription program.
Read More
Insights Shared by Community-based Organizations and Payers
Both sets of interviews explored examples of successful community-based organization-health care Food is Medicine partnerships; systems-level support needed to make community-based organizations more competitive in the Food is Medicine space. Below are key takeaways from the interviews, organized by the main topics discussed.
Community-based Organizations
Characteristics of successful community-based organizations-health care partnerships
- Partnerships that are a natural, rather than a forced, fit
- Partnerships in which partners are in close proximity and champions in their respective spaces
- Food is Medicine initiatives that start with and build on reimbursement from Medicaid, whose beneficiaries are often included in an initiative's intended populationsg to diverse audiences
Putting It All Together

Below are summarized examples of successful community-based organizations' partnerships with health care, systems-level supports to make community-based organizations more competitive in Food is Medicine, and dissemination strategies that emerged across Food & Society's community-based organizations and payer interviews. Case studies presented later in the report will provide deep-dive examples and compelling stories that further elucidate many of these findings.
Read More